Breathing requires the movement of air into and out of the lungs. This is normally accomplished by the diaphragm and chest muscles. A variety of medical conditions can impair the ability of these muscles to accomplish this task. In these medical conditions, external breathing support is required for savings of patient’s life that is called mechanical ventilation.
Mechanical ventilation is a life supportive measure. Mechanical ventilation is provided by mechanical ventilator. Mechanical ventilator is a machine that helps patient breathe when they are not able to breathe enough on their own. The mechanical ventilator is also called a ventilator, respirator, or breathing machine.
Mechanical ventilator is an artificial, external organ that was conceived originally to replace, and later to assist, the respiratory muscles. The primary function of mechanical ventilators is to promote alveolar ventilation to maintain adequate oxygenation or carbon dioxide elimination.
· Mechanical ventilation is a method to mechanically assist or replace spontaneous breathing.
· Mechanical ventilation can be defined as the technique through which gas is moved toward and from the lungs through an external device connected directly to the patient.
· Mechanical ventilation is the use of a machine to take over active breathing for a patient. It is used when a patient can no longer breathe due to injury, illness, or general anesthesia during surgery.
· Mechanical ventilation is the use of a machine called a ventilator or respirator to improve the exchange of air between the lungs and the atmosphere.
· Mechanical ventilator is an automatic machine designed to provide all or part of the work the body must produce to move gas into and out of the lungs. The act of moving air into and out of the lungs is called breathing, or, more formally, ventilation.
The respiratory system can be modelled as a gas exchanger (the lungs) ventilated by a pump. Dysfunction of either, pump or lungs can cause respiratory failure, defined as an inability to maintain adequate gas exchange while breathing ambient air.
Respiratory failure is usually classified as –
1. Lung failure (failure of the lung parenchyma), often termed type 1 failure
2. Pump failure (failure of ventilator function) which is termed type 2 failure
Pump failure
Pump failure primarily results in alveolar hypoventilation, hypercapnia and respiratory acidosis. Inadequate alveolar ventilation may result from a number of causes intrinsically affecting one or more components of the complex pathway that begins in the respiratory centres (pump controller) continues with central and peripheral motor nerves ends with the chest wall, including both the respiratory muscles and all the passive elements that couple the muscles with the lungs.
Alveolar hypoventilation may even be seen in the absence of any intrinsic problem of the pump, when a high ventilation load overwhelms the reserve capacity of the pump. Excessive load can be caused by airway obstruction, respiratory system stiffening (low compliance) or a high ventilation requirement culminating in intrinsic pump dysfunction due to respiratory muscle fatigue.
Lung failure
Lung failure results from damage to the gas exchanger units: alveoli, airways and vessels.
Lung failure involves impaired oxygenation and impaired CO2 elimination depending on a variable combination of Ventilation/perfusion mismatch, True intrapulmonary shunt and increased alveolar dead space.
Lung injury is also associated with increased ventilation requirements and mechanical dysfunction resulting in high impedance to ventilation. Impedance of the respiratory system is most commonly expressed by the quantifiable elements of respiratory system resistance, respiratory system compliance, and intrinsic PEEP (positive end-expiratory pressure).
Pump failure and lung failure rarely occur in isolation, in intensive care patients. Frequently a patient alternates between prevalent pump failure and prevalent lung failure, during the course of their illness.
Pump failure may cause lung failure due to accumulation of secretions, inadequate ventilation and atelectasis. Lung failure may cause pump failure, due to high impedance and increased ventilation requirement.
Mechanical ventilation is instituted -
1) To maintain or improve sufficient ventilation.
2) To provide exact concentration of FiO2.
3) To obtain an adequate ventilation & tissue oxygenation.
4) To Decrease the work of breathing and improve patient’s comfort.
· Post-operative
ü After major abdominal or cardiac surgery
· Respiratory failure
ü ARDS
ü Acute severe asthma
ü Pneumonia
ü Aspiration
ü COPD
ü Smoke inhalation, burns
· Circulatory failure
ü Low cardiac output: cardiogenic shock
ü Following cardiac arrest
ü Pulmonary oedema
· Neurological disease
ü Coma of any cause
ü Status epilepticus
ü Drug overdose
ü Respiratory muscle failure (e.g. Guillain–Barré syndrome, poliomyelitis, myasthenia gravis)
ü Head injury: to avoid hypoxaemia and hypercapnia, and reduce intracranial pressure
ü Bulbar abnormalities causing risk of aspiration (e.g. cerebrovascular accident, myasthenia gravis)
· Multiple trauma
Criteria for institution of ventilatory support:
|
Parameters |
Ventilation indicated |
Normal range |
|
Pulmonary function studies: · Respiratory rate (breaths/min). · Tidal volume (ml/kg body wt) · Vital capacity (ml/kg body wt) · Maximum Inspiratory Force (cm H2O) |
> 35 < 5 < 15 <-20 |
10-20 5-7 65-75 75-100 |
|
Arterial blood Gases · pH · PaO2 (mmHg) · PaCO2 (mmHg) |
< 7.25 < 60 > 50 |
7.35-7.45 75-100 35-45 |
Note - These parameters are used in making judgments about the adequacy of respiratory function.
1. Invasive ventilation – it refers to the administration of ventilatory support with using an invasive artificial airway like endotracheal tube or tracheostomy tube.
2. Noninvasive ventilation (NIV) - refers to the administration of ventilatory support without using an invasive artificial airway.
Negative-Pressure Ventilators
The principle of operation of a negative-pressure ventilator is the flow of air to the lungs is created by generating a negative pressure around the patient’s thoracic cage. The negative pressure moves the thoracic walls outward expanding the intra-thoracic volume and dropping the pressure inside the lungs. The pressure gradient between the atmosphere and the lungs causes the flow of atmospheric air into the lungs. The inspiratory and expiratory phases of the respiration are controlled by cycling the pressure inside the body chamber between a sub-atmospheric level (inspiration) and the atmospheric level (exhalation). Flow of the breath out of the lungs during exhalation is caused by the recoil of thoracic muscles.
The negative-pressure ventilator is a chamber for creating negative pressure around the thoracic walls. One approach has been to make the chamber large enough to house the entire body with the exception of the head and neck. Using foam rubber around the patient’s neck, one can seal the chamber and generate a negative pressure inside the chamber. This design configuration, commonly known as the iron lung, was tried back in the 1920s and proved to be deficient in several aspects. The main drawback was that the negative pressure generated inside the chamber was applied to the chest as well as the abdominal wall, thus creating a venous blood pool in the abdomen and reducing cardiac output.
More recent designs have tried to restrict the application of the negative pressure to the chest walls by designing a chamber that goes only around the chest. However, this has not been successful because obtaining a seal around the chest wall is difficult.
Negative-pressure ventilators also made the patient less accessible for patient care and monitoring. Further, synchronization of the machine cycle with the patient’s effort was has been difficult and they are also typically noisy and bulky. These deficiencies of the negative pressure ventilators have led to the development of the positive-pressure ventilators.
Positive-Pressure Ventilators
Positive pressure ventilation was a result of the polio epidemic in 1955, when the demand for mechanical ventilation exceeded the available number of negative pressure ventilators. There was such a shortage in Sweden that medical students worked in 8-hour shifts, manually ventilating polio patients. The Emerson Company in Boston developed the positive pressure ventilator, which was first used at Massachusetts General Hospital. It was an immediate success, and launched a new era of intensive care medicine.
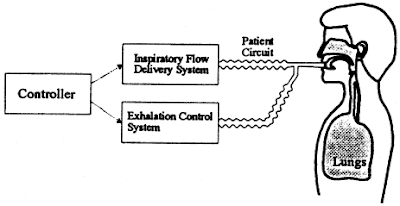
Positive pressure ventilators require an artificial airway (endotracheal or tracheostomy tube), and use positive pressure to force oxygen into a patient’s lungs. Inspiration can be triggered either by the patient or the machine. During inspiration, the inspiratory flow delivery system creates a positive pressure in the tubes connected to the patient airway, called patient circuit, and the exhalation control system closes a valve at the outlet of the tubing to the atmosphere. When the ventilator switches to exhalation, the inspiratory flow delivery system stops the positive pressure and the exhalation system opens the valve to allow the patient’s exhaled breath to flow to the atmosphere.
The use of a positive pressure gradient in creating the flow allows treatment of patients with high lung resistance and low compliance. As a result, positive-pressure ventilators have been very successful in treating a variety of breathing disorders and have become more popular than negative-pressure ventilators.
There are four types of positive pressure ventilators:
1. Volume cycled
2. Pressure cycled
3. Flow cycled
4. Time cycled
1. Volume-cycled ventilators are designed to deliver a preset tidal volume, then, allow passive expiration. This is ideal for patients with bronchospasm since the same tidal volume is delivered regardless of the amount of airway resistance. This type of ventilator is the most commonly used in critical care environments.
2. Pressure-cycled ventilators deliver gases at preset pressure, then, allow passive expiration. The benefit of this is a decreased risk of lung damage from high inspiratory pressures. The disadvantage of these ventilators is that the patient may not receive the complete tidal volume if he or she has poor lung compliance and increased airway resistance. This type of ventilation is usually used for short-term therapy (less than 24 hours). Some ventilators have the capability to provide both volume-cycled and pressure-cycled ventilation. These combination ventilators are also commonly used in critical care environments.
3. Flow-cycled ventilators deliver a breath until a preset flow rate is achieved during inspiration.
4. Time-cycled ventilators deliver a breath over a preset time period. These aren’t used as much as the volume-cycled and pressure-cycled ventilators.
Types of Ventilators (biased on breathing frequency)
Biased on breathing frequency, there are two classes of ventilators.
Conventional ventilators - Conventional ventilators produce breathing patterns that mimic the way we normally breathe (ie, at rates our bodies produce during our usual living activities: 12 - 25 breaths/min for children and adults; 30 - 40 breaths/min for infants). These are called conventional ventilators and their maximum rate is 150 breaths /minute. The vast majority of ventilators used in the world provide conventional ventilation. This employs breathing patterns that approximate those produced by a normal spontaneously breathing person.
High frequency ventilators - High frequency ventilators produce breathing patterns at frequencies much higher than we would or could voluntarily produce for breathing - called high frequency ventilators. These ventilators can produce rates up to 15 Hz (900 breaths/minute).
Books
1. Brunner LS, Suddarth DS, Smeltzer SCO. Brunner & Suddarth’s textbook of medical-surgical nursing. Philadelphia: Lippincott Williams & Wilkins; 2008. Page No. 739-754
2. Nettina SM, Lippincott Williams & Wilkins. Lippincott manual of nursing practice. Philadelphia: Wolters Kluwer Health : Lippincott Williams & Wilkins; 2010. Page No. 255-267
3. Longo DL, Harrison T. Harrison’s principles of internal medicine. New York, N.Y., [etc.]: McGraw-Hill Medical; 2012. Page No-
4. Colledge NR, Walker BR, Ralston S, Davidson S. Davidson’s principles and practice of medicine. Edinburgh; New York: Churchill Livingstone/Elsevier; 2010. Page No. 194-198
Web page
1. Adult Invasive Mechanical Ventilation.pdf [Internet]. [cited 2012 May 28]. Available from: http://www.mecriticalcare.net/downloads/mv/AdultInvasiveMechanicalVentilation.pdf
2. Adult Ventilation Management Online Nursing Continuing Education Course [Internet]. [cited 2012 May 28]. Available from: http://www.corexcel.com/courses/Vent_Web_Handout.pdf
3. Critical Care Nursing Theory - Mechanical ventilation [Internet]. [cited 2012 May 28]. Available from: http://www.philadelphia.edu.jo/academics/abatiha/uploads/Mechanical%20ventilation.pdf
4. Patient Education Series American Thoracic Society Mechanical Ventilation [Internet]. [cited 2012 May 28]. Available from: http://patients.thoracic.org/information-series/en/resources/mechanical-ventilation.pdf
5. Core Topics in Mechanical Ventilation [Internet]. [cited 2012 May 28]. Available from: http://www.csen.com/vent.pdf
6. Fundamentals of Mechanical Ventilation [Internet]. [cited 2012 May 28]. Available from: http://www.ventworld.com/resources/pdf/vwchat.pdf
7. Mechanical Ventilation Critical Care Clinic [Internet]. [cited 2012 May 28]. Available from: http://www.scribd.com/doc/25317501/Mechanical-Ventilation-Critical
8. Mechanical Ventilation for Nursing.ppt [Internet]. [cited 2012 May 28]. Available from: http://wwwappskc.lonestar.edu/programs/respcare/Missy%27s%20website/Mechanical%20Ventilation%20for%20Nursing.ppt
9. Mechanical ventilation Skills and techniques Update 2011 [Internet]. [cited 2012 May 28]. Available from: http://pact.esicm.org/media/Mechanical%20vent%201Feb2011%20final.pdf
10. Mechanical Ventilation.ppt [Internet]. [cited 2012 May 28]. Available from: http://home.cmcvellore.ac.in/upcoming/CME/ppt/Mechanical%20Ventilation.ppt
11. Mechanical Ventilation.ppt [Internet]. [cited 2012 May 28]. Available from: http://www.mcgill.ca/files/emergency/Mechanical_Ventilation.ppt
12. Modes of Ventilation ppt [Internet]. [cited 2012 May 28]. Available from: http://faculty.mdc.edu/pslocum/RET%202284%20Mod%203.0%20Modes%20of%20Ventilation.ppt
13. Nursing care of the mechanically ventilated patient: What does the evidence say? pdf [Internet]. [cited 2012 May 28]. Available from: http://eprints.qut.edu.au/33268/1/coyerdarticle%5B1%5D.pdf
14. Nursing Care Of The Ventilated Patient [Internet]. [cited 2012 May 28]. Available from: http://intensivecare.hsnet.nsw.gov.au/five/doc/nurse_care_V_swahs.pdf
15. Principle of Mechenical Ventilation [Internet]. [cited 2012 May 28]. Available from: http://www.cmia.org/images/ventilation.pdf
16. Chapter 82 - Mechanical Ventilation [Internet]. [cited 2012 May 28]. Available from: http://kemt.fei.tuke.sk/Predmety/KEMT537_LE/_materialy/09-Biomedical%20Engineering%20Handbook,%20The%20-Volumes%201%20%26%202/ch082.pdf
17. respiratory-failure-mechanical-ventilation.pdf [Internet]. [cited 2012 May 28]. Available from: http://www.thoracic.org/clinical/critical-care/clinical-education/respiratory-failure-mechanical-ventilation.pdf
18. Advances In Mechanical Ventilation [Internet]. [cited 2012 May 28]. Available from: http://www.newportnmi.com/FileDownloads/GENERAL-tobinmechvent.pdf
19. Standard of Practice: Care of the Mechanically Ventilated Patient [Internet]. [cited 2012 May 28]. Available from: http://www.cc.nih.gov/ccmd/cctrcs/pdf_docs/Ventilator%20Management/01-SOP-Carof%20the%20Mech.pdf
20. Invasive Mechanical Ventilation ppt [Internet]. [cited 2012 May 28]. Available from: http://home.cmcvellore.ac.in/upcoming/CME/ppt/Invasive%20Mechanical%20Ventilation.ppt
21. Management of the mechanically ventilated. Patient in the emergency department [Internet]. [cited 2012 May 28]. Available from: https://notendur.hi.is/thorsj/tasota/ED_MV.pdf
22. Mechanical Ventilation: A Review and Update for Clinicians [Internet]. [cited 2012 May 28]. Available from: http://seminmedpract.com/pdf/hp_dec99_vent.pdf
23. How to Withdraw Mechanical Ventilation [Internet]. [cited 2012 May 28]. Available from: http://www.aacn.org/WD/CETests/Media/CI1841.pdf
24. Mechanical ventilation: Weaning and extubation [Internet]. [cited 2012 May 28]. Available from: http://www.opus12.org/uploads/O12-SCI-V01-N02-P13.pdf
25. Withdrawal of Ventilatory Support from the Dying Adult Patient [Internet]. [cited 2012 May 28]. Available from: http://jso.imng.com/jso/journal/articles/0203283.pdf






Perfect knowledgeable blog.
ReplyDeleteThis blog information is really helpful.
ventilator gallatin nashville hendersonville
I am curious to find out what blog platform you are utilizing? I'm having some minor security problems with my latest blog and I would like to find something more risk-free. Do you have any suggestions? ppe equipment australia
ReplyDeleteApne Bikul shahi Samjhaya ki Ventilator kya hota hai
ReplyDeleteBuy Tadalafil 10mg Tablet Lowest Price
ReplyDeleteBuy Tadaga 10mg Tablet
Mantram Nursing Academy’s NORCET online coaching in Ambala, Haryana offers live interactive sessions, experienced faculty, and regular assessments to help students prepare efficiently for the NORCET exam.
ReplyDeleteNORCET Online Coaching in Ambala Haryana